- Published on
The Lifecycle of an Appeal (Part 5)
- Authors

- Name
- Mike Gartner, PhD
Recap
This is part 5 of a multi-part post walking through an appeal of a coverage denial for Adalimumab level testing. We previously submitted a first internal appeal of the decision.
The Initial Response
On June 10, I received an official response from Aetna regarding my appeal. You may not be shocked to hear that not only did Aetna decide to stick to their initial decision of denying my coverage request, and thereby maintain higher profits for themselves, they also chose to just not respond to a single piece of detail in my appeal.
Here is the full content of their justification for upholding the denial in the face of the new evidence:
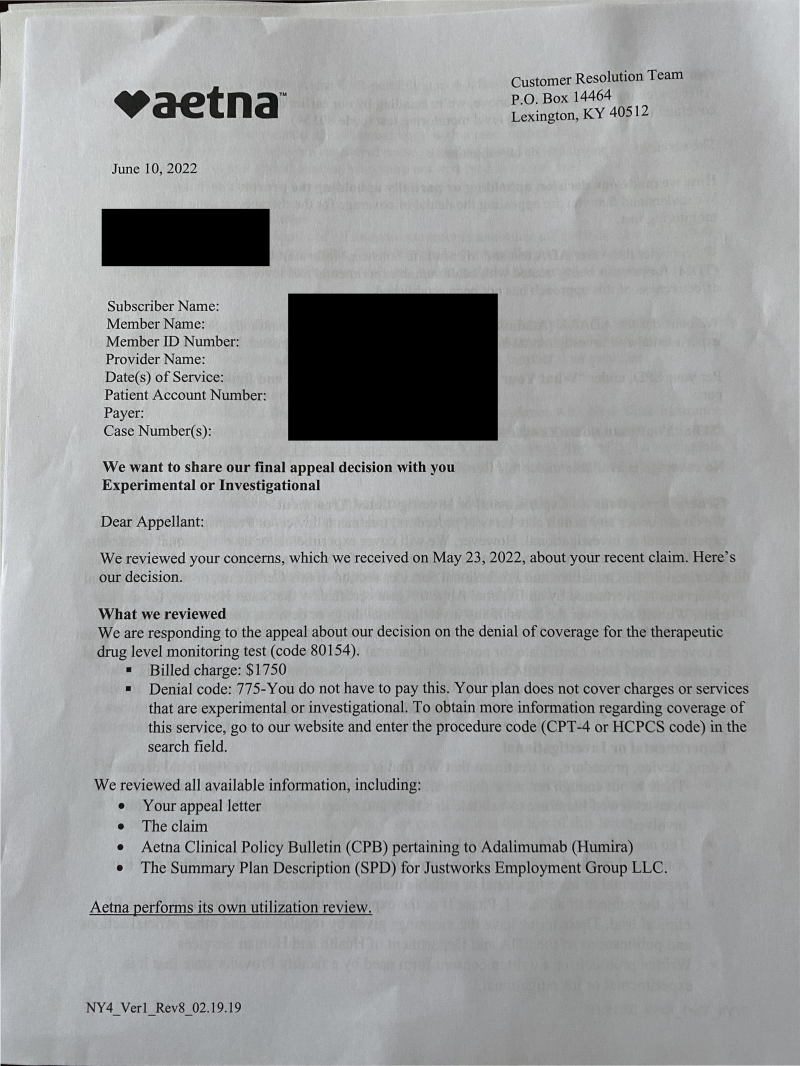
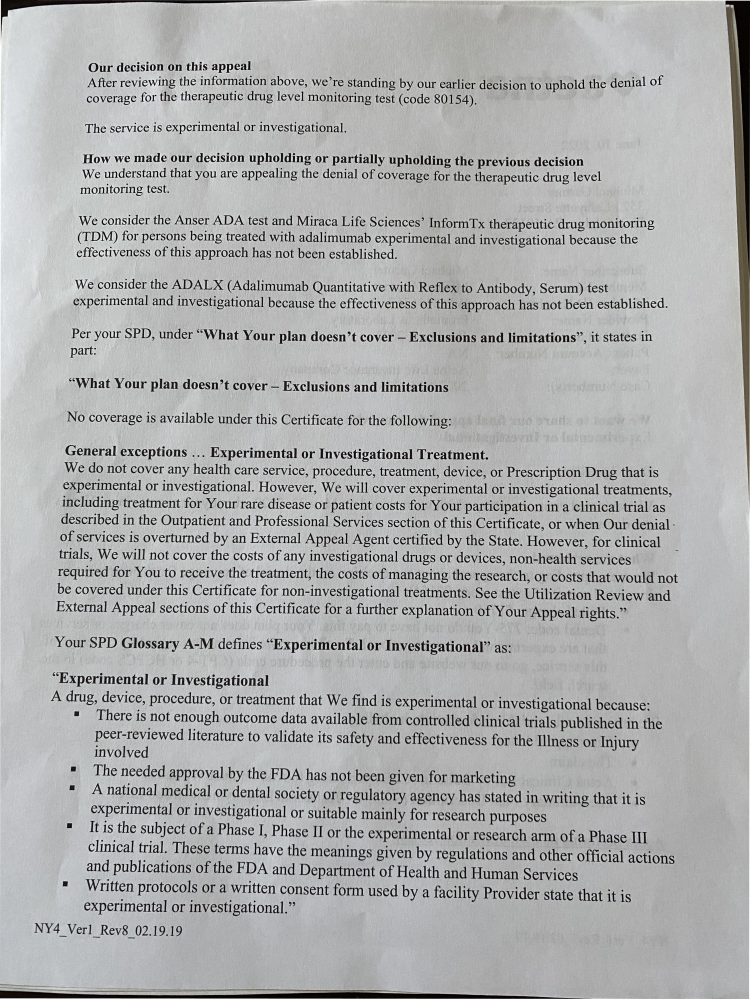
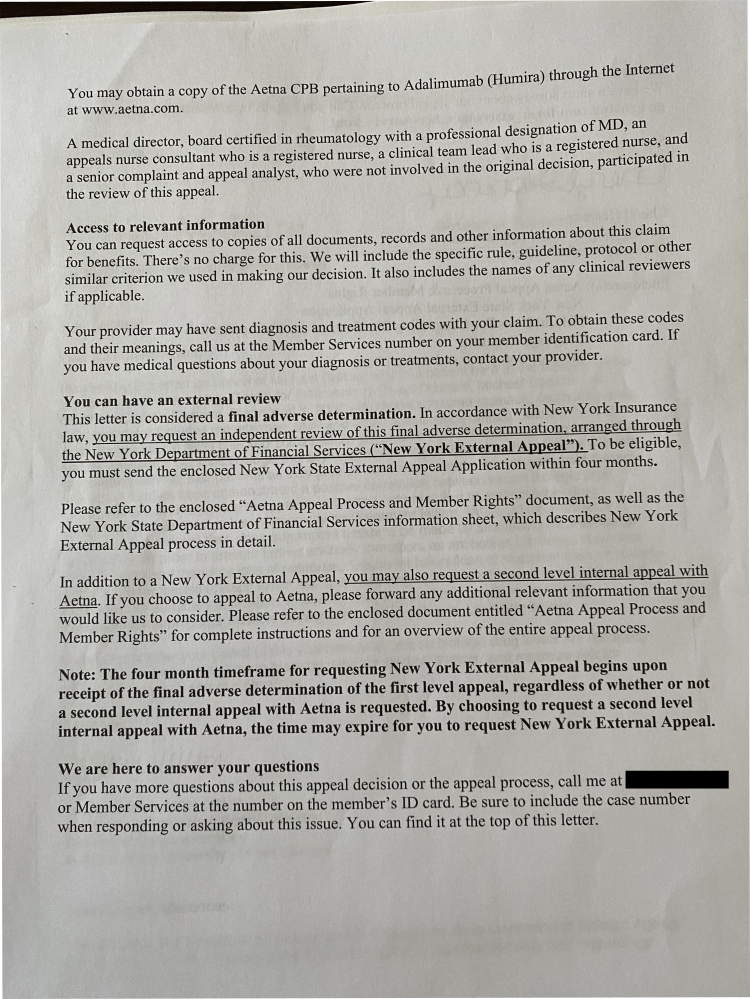
Figure 1.
The response to my appeal.
If you squint and don't read the content, it almost looks like they are making a compelling argument for why my appeal is not merited. But if you choose to actually read it, and cross reference with the initial coverage denial determination, you'll see that all they've done is repeated pertinent sections of the plan documents. This is exactly what we addressed point by point in the appeal, but none of our evidence is being addressed. This is the corporate equivalent of "I'm not listening". I guess they were hoping we just wouldn't read this letter carefully?
There's something to be said about those who are incapable of changing their viewpoints in the face of new data. I'll leave it unsaid.
Next Steps
While the reaffirmation of the denial is disheartening, it's good to keep in mind that this is completely expected behavior for a corporation trying to maximize it's profits. We should not expect them to self police themselves in good faith. Luckily, there is a system of recourse in place to make this process less blatantly stacked against consumers, at least for those fortunate enough to have the time and resources to get this far. That recourse is the external appeal.
Once consumers have exhausted a certain number of available appeal avenues with insurers themselves, insurers are required to abide by a process in which consumers can submit a final appeal to an external review board, consisting of reviewers employed by a third party organization. The external review board decides whether or not the original adverse decision should be upheld, and insurers are required by law to act in accordance with any decision to overturn a denial made by the board.
The exact rules for when a consumer can proceed with an external review vary by state, but typically one must complete one or two levels of internal appeals with their insurer before this recourse is available. To learn more about how the rules vary by state, you can check out the relevant page for your state on our site here1.
Luckily in the case at hand Aetna includes in their letter that this decision constitutes their "final adverse determination", which means that this denial is now immediately eligible to be submitted to an external review board.
It is insane that consumers must first exhaust some number of internal appeal processes before being afforded the opportunity to have their denials investigated by an unbiased third party. This is a huge barrier in the form of time and red tape that effectively precludes many people from ever getting an impartial review.
I'm tired2 so we'll end this post here, but tune in next time as we walk through the process of gathering more requisite documents for yet another correspondence about the idiocy of this denial. Ooo wee.
Footnotes
Currently, you'll need to make a free acount to access the linked page on persius.org; there's no cost, no card required, no emails, and you can even use a fake email and name if you really want, since we don't verify anything. The reason we currently limit some data to account holders is solely because everything we provide is free, but hosting is not. We'd like to make maintaining these resources our day jobs, but until then, requiring account creation provides one means of monitoring aggregate usage, limiting costs due to automated internet traffic, and testing utility of resources we provide; also, number of accounts is a metric that allows us to prove to potential funders that people find utility in what we are providing. If you'd rather not make an account on our site for any reason, you can find all the same info by digging around online, starting at healthcare.gov. You can also just email me personally, and I'd be happy to share any information with you whether or not you want to create an account. ↩
Aren't we all tired from dealing with this bullshit? ↩
