- Published on
The Lifecycle of an Appeal (Part 2)
- Authors

- Name
- Mike Gartner, PhD
Recap
This is part 2 of our multi-part post walking through an appeal of a coverage denial for Adalimumab level testing. Just like in dealing with grief associated with many things other than insurance issues, one of the first stages of the appeal process involves denial.
The Denial
I ended the last post recalling a feeling of relief when I found out the original claim for coverage had never been submitted to my insurer, and that the third party lab would now be submitting such a claim on my behalf. Well, the joke was on me, because my old insurer promptly responded by denying my claim for coverage for the drug level test. You can see the main content of the letter in it's full glory below, annotated with some boxes we'll get to later.
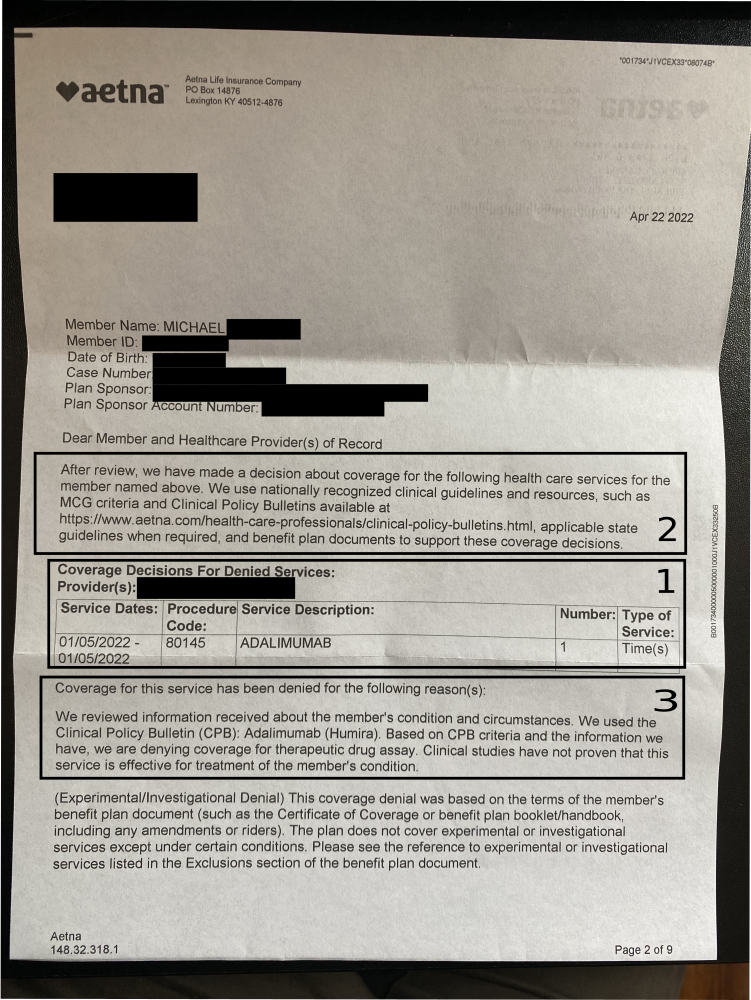
Figure 1.
An annotated page of the denial letter, detailing member and coverage credentials, the denied service, and the denial rationale. Some personal and company information is redacted.
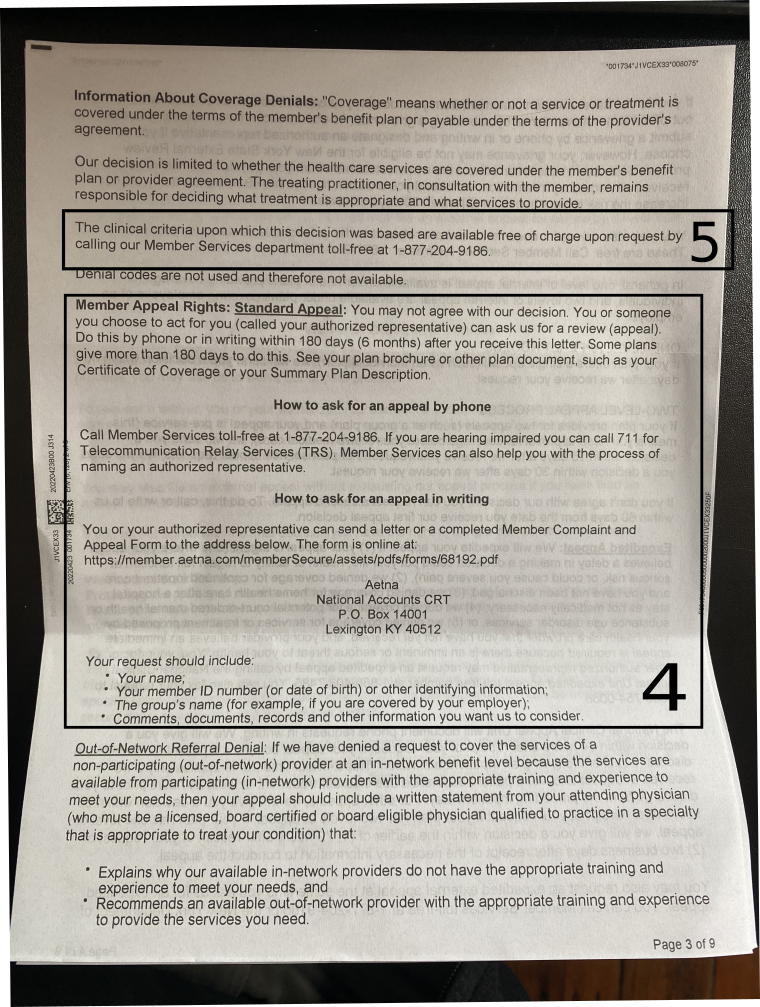
Figure 2.
Another annotated page of the denial letter, detailing appeal logistics.
I want to use this coverage denial as an opportunity to walk through the process of writing an appeal letter, and point out some tips about what to look out for, what to include, and how to frame the process.
To prepare for appealing the denial, there are four key questions we'll need to answer:
- What services or treatments were denied coverage?
- What were the procedures and sources used to inform the denial?
- What specific rationale was given for this denial, if any?
- What is the requisite procedure for appealing this denial?
Question 1 is something you may have to ascertain from somewhere other than the letter, but the letter may provide a technical summary of the situation from the insurer's perspective. In my case, this is addressed in Box 1 by the specified procedure code, and a description of the service. It will be helpful in my case to supplement this procedure code, which google says is for "Therapeutic Drug Assays", with our knowledge that it corresponds to a level test for the drug Adalimumab.
Question 2 is addressed by Box 2 in the image. It states:
We use nationally recognized clinical guidelines and resources, such as MCG criteria and Clinical Policy Bulletins available at https://www.aetna.com/health-care-professionals/clinical-policy-bulletins.html, applicable state guidelines when required, and benefit plan documents to support these coverage decisions.
Here we learn that in addition to plan benefit documents, which will of course always be one source utilized in coverage decisions, Aetna claims they use nationally recognized guidelines, and state guidelines, to inform their decisions, and lists MCG criteria and Clinical Policy Bulletins (CPBs) as two examples of such. If you don't see any explanation of the general procedures used to determine claim decisions in your denial letter, look in your plan benefit documents for these details instead. They should be detailed in at least one of those two places.
Question 3 is addressed by Box 3 in the image. It gives a more specific explanation for the denial:
We used the clinical policy bulletin (CPB): Adalimumab (Humira). Based on CPB criteria and the information we have, we are denying coverage for therapeutic drug assay. Clinical studies have not proven that this service is effective for treatment of the member's condition.
Finally question 4 is addressed by Box 4 in the second image. It informs us of how we will need to proceed with submitting an appeal. Such information should also be contained in your plan benefit documents, so check there if no information is given in the denial letter for next steps.
Box 5 in the second image is highlighted because it is comically absurd. Aetna is inviting you to call an insurance customer support line, probably wait on hold for a long while, get on the line with someone who likely will have no idea what clinical criteria you are referring to, and then, supposing they do actually know and have access to the clinical criteria they are supposed to provide to you, they'll what....send you a bunch of research papers by mail? Recite to you the clinical criteria established via studies, on the phone? Read you the urls or citations for the papers they used to establish their decision?
A useful thing to do would be document the explicit clinical criteria used to make this decision, and include references to the relevant sources, in the denial letter itself, so that all of the information necessary to write an appeal is accessible to the patient in a relatively self-contained way. Instead we have numerous layers of obfuscation.
But don't worry! If you were concerned about the cost of hearing the clinical criteria they used to deny your treatment via phone, it's on the house. It's almost like you're coming out ahead; just avoid thinking about the time you have to spend on hold, your $1000/month premium, and the potentially enormous out of pocket costs for the denied treatment. Such generosity 😂
Some Venting
Let's take a moment to vent about this letter, before getting back to being productive. In my experience, venting about frustrating interactions with health insurance is the only way to retain some semblance of sanity. This letter is ridiculous for numerous reasons, and seems likely to have been written by someone who is incompetent, malicious, a computer, or perhaps none of those but who is working for someone who is incompetent or malicious (or I guess a computer?!).
First of all, there's some obfuscation and conflation going on in this letter. The letter confusingly describes the service being denied as "Adalimumab" (that's the drug itself), while the CPT code 80145 correctly indicates that the service in question is actually a test assay to test for Adalimumab levels. Also we can note the "type of service" is listed as "time", which seems off; even if for some reason these are technically the correct descriptions, their meaning is by no means clear in this context, and they should therefore be explained to the consumer to whom the letter is addressed.
The lack of clarity comes into play in the denial statement itself. The denial claims that clinical studies have not proven that this service is effective for the treatment of the member's condition. Presumably they are referring to the particular drug level test I actually received, but this isn't entirely clear from their wording. They described the service as "Adalimumab", and the type of service as "time", while the CPT code indicates a drug level assay, so their reference to "this service" now allows for a large range of possible interpretations, and it is more likely they can successfully defend at least one of those interpretations if they are challenged. In addition, the particular wording they use says clinical studies have not proven the service is effective for the member's condition. Clinical studies rarely prove anything to a without-a-doubt level (because sample sizes are small, and factors at play are myriad), and even when they do, study authors are cognizant of the role of statistics in their work so will virtually never use language like "prove" when summarizing the results of a clinical study. For this reason, even if every single reference in Aetna's own policy documents found that level testing of Adalimumab was effective in treating a condition, if they avoided conclusive language like "prove", Aetna could technically defend their denial rationale. They've given themselves a lot of outs, even if they were blatantly misrepresenting the facts here1.
Second, what this statement effectively claims is something like "The rationale for the denial is very legitimate, based on lots of science and reputable sources, but we're not going to explicitly tell you here which of those sources or which science we really think backs up our claim. Instead we are going to provide a laundry list of reputable sources (e.g. MCG criteria, with no link to particular criteria, and an internal CPB document, which itself has 187 references listed) and let you try to deduce how (if at all) these sources back up our actual rationale for the denial at hand." At absolute best, with the most generous interpretation of why this reponse is the way it is, this is an incredibly lazy response for a decision which could have severe consequences for the recipient2. Another possibility is this denial strategy has nothing to do with laziness and everything to do with a calculated effort to maximize profit. The clearer and more transparent denials are, the easier they will be to appeal successfully, which would directly affect insurer profits.
Remind me next I'm involved in a technical argument to use this timeless strategy.
My argument for my point is as follows. I've read all of the relevant scientific papers on the technical topic at hand, and consulted all of the experts, and these sources collectively indicate that what I've said is correct. Here is a list of hundreds of such papers and experts for you to peruse. Good day.
Footnotes
To be clear, I'm not saying they are misrepresenting facts here. At this point in this multi-post series, the veracity of their claims is yet to be determined. Stay tuned for the surprising twist ending! ↩
To be clear, I am fortunate to say that is not the case for me in this instance, and the consequences for me here are fortunately low stakes. ↩
